Want to treat diseases with more precision? Use big data
Americans spent $3.2 trillion dollars on healthcare in 2015, the most recent year for which the Centers for Medicare and Medicaid Services have complete data. That's almost $10,000 per man, woman, and child in the country — and the numbers are growing. Healthcare spending increased 5.8% year-over-year in 2015. By 2020, leading healthcare IT company Leidos estimates that healthcare spending will comprise 20% of U.S. GDP.
With America's aging population, and more seniors entering the Medicare system daily, costs are almost certain to continue to rise in the near term. What's essential now, for healthcare providers, for insurers and government — and most importantly for patients — is to begin bending the cost curve.
Using big data to process the treasure trove of digitized health information (electronic health records, or EHR) into relevant, actionable knowledge can lead to "precision medicine," a way to treat patients more efficiently and at lower cost. Precision medicine is one way to help flatten the cost of healthcare, and Leidos is actively involved in this area.
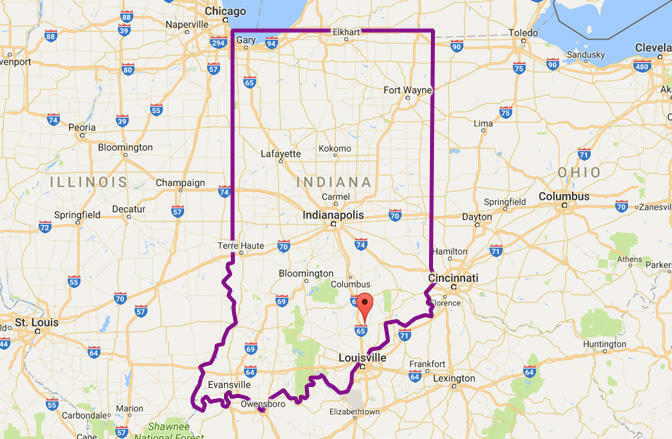
Tackling an HIV outbreak in Indiana
In late 2014, an HIV infection epidemic spread across tiny Scott County, Indiana, baffling healthcare providers who had previously seen little sign of the disease in the county. The U.S. Centers for Disease Control (CDC) quickly went to work and applied Collaborative Advanced Analytics & Data Sharing (CAADS), a Hadoop-based big data software developed by Leidos.
Officials used CAADS to analyze disparate data points collected from the county health system, the CDC's own internal data, and publicly available information. The software utilizes a single, secure interface (without personally identifiable information) and requires no coding skill to use. With CAADS, the CDC was able to rearrange multiple data points from multiple sources so that they made sense, and identify HIV outbreak clusters, geographic factors, epidemiological patterns, and drug resistance.
Their conclusion: Opioid drug users within the county were sharing needles. Previously, this practice had resulted in widespread cases of hepatitis C infection within the group. Once HIV was introduced into the population, it quickly spread.
Leidos principal scientist Ryan Weil estimates that use of CAADS cut the amount of time needed to figure out what was going on "by a factor of six." Then, utilizing the machine learning function incorporated into CAADS, the CDC was able to generate recommendations on how to interrupt the spread of HIV. CAADS permitted Leidos to track "social networks with the data," to "fuse" these findings with other data, and come up with recommendations: Declare a public health emergency, launch a public education campaign, provide substance abuse counseling and treatment, and set up syringe exchanges.
By mid-2015, the spread of HIV in Indiana had slowed. Not only did CAADS assist the CDC in containing the outbreak in Scott County — data generated during the crisis alerted the agency to the kinds of factors that need to be monitored for early warning against similar crises. The CDC has transmitted this knowledge to alert "state, local, and territorial health departments" of what to look for, decreasing the likelihood of similar outbreaks in the future.
A revolution in pharmacogenomics
Current methods for treating cancer — and indeed most illnesses — follow a "one-size-fits-most" process, applying established treatments that seem to work well for most people, one after another, to an individual patient until one of the approaches works. It almost goes without saying that this is a suboptimal way to treat disease. Scientists now have the ability to collect data on which treatments work best for specific genetic profiles, and apply these specific treatments to individuals with the appropriate profiles.
Leidos is taking the lead in this new field of precision medicine through "biopharmaceutical concept prototyping." In oncology, for example, Leidos employs big data methods to predict which treatments will work best on tumors based on the individual patient's genetic traits.
In this field of pharmacogenomics, Leidos models how specific genetic patterns are likely to respond to specific cancer medications. At the U.S. Department of Veterans Affairs, Leidos is helping integrate genomic and clinical data, and then using computer modeling to see how various medications will affect patients with a given set of genomic attributes. Such models can also help to predict diseases caused by genetic abnormalities before they strike. This permits VA doctors to begin preventative care plans and early screenings to reduce the need for more drastic — and expensive — treatments later on.
Pharmacogenomics also holds the potential — when combined with big data analyses of the most common patient genetic profiles — to more efficiently guide research into new cancer-fighting drugs to target the largest patient populations at the lowest cost.
In HIV, in cancer, and in a host of other diseases, Leidos is using big data to transform how healthcare providers approach and treat healthcare crises — on a personal level and at the larger level of treating the population. More and more often, they're finding that whether you need a "hacksaw" or a "scalpel," big data can provide the right tool to treat the disease.